At Tech Hub Solutions, we provide comprehensive medical billing services to healthcare providers, ensuring faster reimbursements, reduced claim denials, and seamless revenue management.
Medical Billing & Coding
Accurate & Compliant Medical Coding:
Medical coding is the backbone of a successful billing process. At Tech Hub Solutions, our certified coders ensure the accurate assignment of CPT, ICD-10, and HCPCS codes, reducing the chances of claim denials due to coding errors.
Error-Free Billing Submissions:
We use advanced billing software to process medical claims with high accuracy. Our system cross-verifies every claim for missing information, incorrect codes, or compliance issues, ensuring timely approvals from insurance providers.
Regulatory Compliance & HIPAA Standards:
Our billing and coding services follow HIPAA regulations and industry standards, ensuring that all patient data remains secure and confidential while maximizing your revenue potential.

Claims Submission & Follow-up
Fast & Efficient Claims Processing:
We handle both electronic and paper claim submissions, ensuring that your claims are sent to the insurance providers without delays or errors. Our team double-checks every detail before submission, minimizing the risk of claim rejections.
Regular Follow-ups for Faster Approvals:
Denied claims can be frustrating and time-consuming. Our experts conduct regular follow-ups with insurance companies, ensuring quick resolution of pending claims and accelerating your cash flow.
Appeals & Claim Resubmissions:
In case of claim denials, we identify the root cause, correct errors, and resubmit claims with the necessary documentation. This results in higher approval rates and reduced revenue loss for healthcare providers.
Insurance Eligibility Verification
Ensuring Patients Are Covered:
Many claims are denied due to insurance coverage issues. We provide a real-time insurance verification service, ensuring that patients have active coverage before services are provided.
Accurate Benefit & Deductible Information:
Our team contacts insurance providers to verify details like deductibles, co-pays, coverage limits, and out-of-pocket expenses, preventing claim issues later in the billing cycle.
Reducing Claim Denials Due to Eligibility Errors:
By verifying insurance before appointments and procedures, we reduce rejected claims and payment delays, helping you focus on patient care rather than billing disputes.

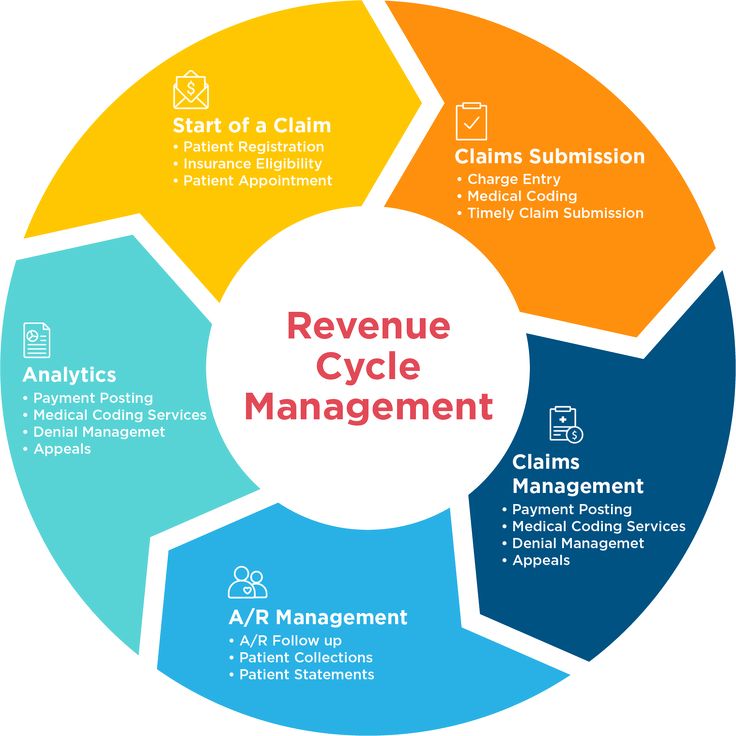
Revenue Cycle Management (RCM)
Optimizing Your Billing Process:
Effective revenue cycle management is crucial for the financial health of your practice. We provide end-to-end billing solutions, from patient registration to final payment collection, streamlining the entire process.
Tracking & Managing Outstanding Payments:
Our system keeps track of pending claims, unpaid invoices, and outstanding balances, ensuring that payments are collected on time and that your revenue remains stable.
Financial Reporting & Insights:
With detailed reports on cash flow, claim success rates, and revenue analytics, we help healthcare providers make informed financial decisions for business growth.
Denial Management & Appeals
Identifying the Cause of Denied Claims:
When an insurance provider denies a claim, we conduct a thorough analysis to determine the exact reason, whether it's a coding error, missing information, or eligibility issue.
Fast & Efficient Claim Resubmissions:
Once we identify the issue, we correct the claim and resubmit it with proper documentation, ensuring a higher approval rate on the second attempt.
Negotiation & Dispute Resolution:
For complex denials, our team works directly with insurance companies to resolve disputes, ensuring that you receive maximum reimbursements with minimal delays.

Ready to Optimize Your Billing Process?